Overview
Two metrics show up repeatedly throughout Marketscape - % Readmitted and % Hospitalized. (readmissions and hospitalizations.) Each of these metrics is a strong indicator of the performance of a hospital or post-acute care provider.
30 days
The reference period for hospitalization and readmission is described in the table header wherever the metric appears. A patient can be admitted to a hospital at any time and there are important reference events or periods that are important to keep in mind:
- Was the patient admitted to a hospital within 30 days of discharge from an inpatient facility? If so, that is a readmission and would tally against the organization readmission metric.
- Was the patient receiving post-acute care at the time they were admitted? If so, that readmission or hospitalization would be counted in the metric for the selected post-acute facility.
- Was the patient admitted to a hospital during their post=acute stay or within 30 days of discharge from post-acute care? If so, this event is counted in the hospitalization metric whether there was a prior inpatient stay within 30 days or not.
Readmission
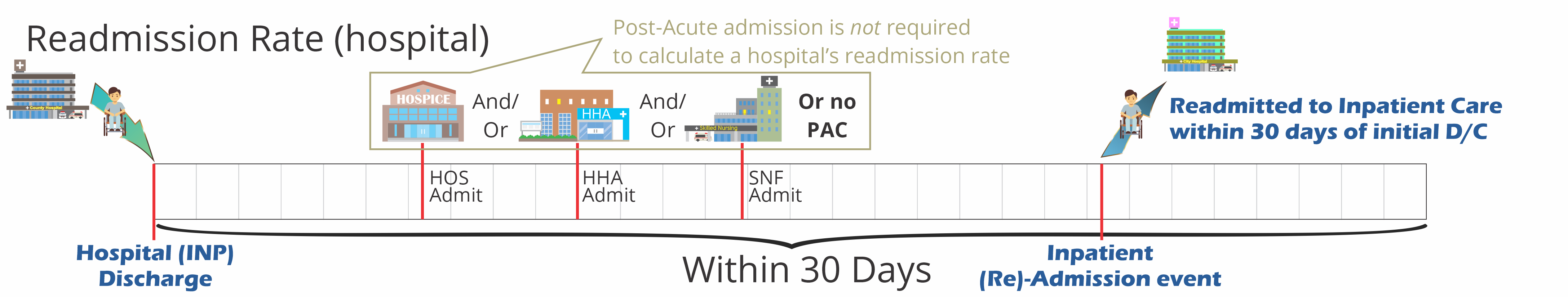
A readmission is a care event where a patient is admitted to any inpatient stay within 30 days of being discharged from an inpatient stay. Like this: INP D/C ![]() INP (RE)Admission within 30 days.
INP (RE)Admission within 30 days.
The Trella Health Readmission Rate is a percentage measurement of readmissions for a select population. This rate can be calculated for either hospitals or post-acute agencies.
![]() You will find Readmission Rates under a lot of names: 30 Day Readmission Rate, Trended Readmit Rate, Readmit Rate, Readmit, % Readmitted: 30 days, or Readmit OR Hospitalization +30 Rate.
You will find Readmission Rates under a lot of names: 30 Day Readmission Rate, Trended Readmit Rate, Readmit Rate, Readmit, % Readmitted: 30 days, or Readmit OR Hospitalization +30 Rate.
![]() For more information, see Readmission Rates.
For more information, see Readmission Rates.
Hospitalization
Although this definition is sometimes adapted to match which facility in the definition is the focus of the metric, the basic definition for % Hospitalized: + 30 days is: The agency’s two year overall rate of hospitalization (where this agency’s patients were admitted to a short-term acute stay during a home health services episode (includes transfers) OR within 30 days of Home Health discharge).
![]() It is a good idea to view the column definitions in the header of each column to identify the specific focus of the hospitalization metric.
It is a good idea to view the column definitions in the header of each column to identify the specific focus of the hospitalization metric.
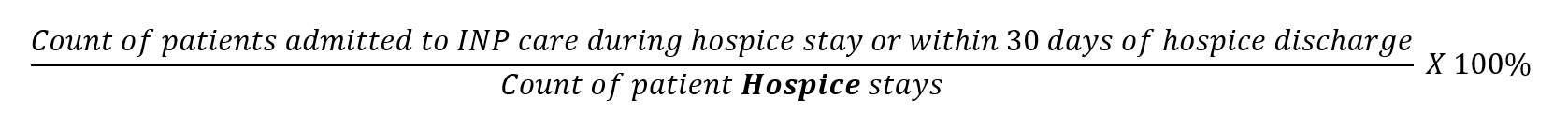
![]() Remember that this metric counts all hospitalizations; the absence or presence of a prior inpatient stay and inpatient discharge has no bearing on this metric.
Remember that this metric counts all hospitalizations; the absence or presence of a prior inpatient stay and inpatient discharge has no bearing on this metric.